Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterized by inflammation in the large intestine and rectum. While the exact cause of UC is still not fully understood, recent research has increasingly pointed to the gut microbiome as a key player in both the development and management of the disease. This article delves into the intricacies of the microbiome’s role in UC, highlighting beneficial bacteria, their nutritional support, and the impact of specific foods and supplements on maintaining a healthy gut environment.
Understanding the Gut Microbiome
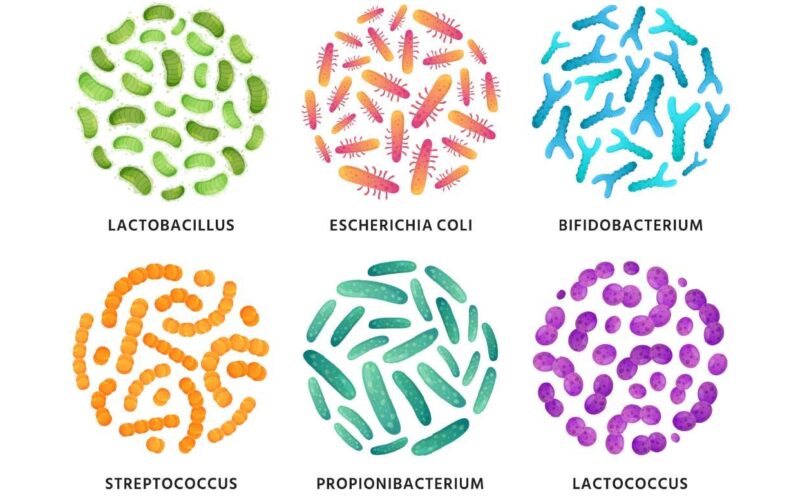
The human gut microbiome is a complex ecosystem made up of trillions of microorganisms, including bacteria, fungi, viruses, and protozoa. In a healthy individual, these microorganisms exist in a balanced state, contributing to various essential functions such as digestion, vitamin production, and immune system regulation. However, in UC patients, this balance is often disrupted — a condition known as dysbiosis — which can exacerbate the immune response and inflammation in the colon.
Beneficial Bacteria and Ulcerative Colitis
Research in the field of gastroenterology has increasingly emphasized the significant role of the gut microbiome in maintaining intestinal health and managing disorders such as Ulcerative Colitis (UC). This body of research has identified specific strains of bacteria that are not only beneficial for overall gut health but also offer potential for mitigating the symptoms associated with UC. Understanding the functions and benefits of these key bacteria can provide insights into how dietary adjustments and probiotic supplements might be utilized to manage UC more effectively.
Key Beneficial Bacteria for Ulcerative Colitis
Lactobacillus
The Lactobacillus genus comprises a variety of bacteria known primarily for their role in fermenting lactose and other sugars into lactic acid. This production of lactic acid is crucial as it helps lower the pH in the gut, creating an environment that is less hospitable to pathogenic bacteria which prefer a more neutral pH. Moreover, specific strains of Lactobacillus play a pivotal role in enhancing the gut barrier function. This barrier is vital for preventing pathogens and toxins from leaking into the body, a condition commonly referred to as “leaky gut,” which can exacerbate inflammatory responses and UC symptoms.
Beyond this, Lactobacillus strains are involved in modulating the body’s immune response, helping to reduce gut inflammation. For instance, Lactobacillus rhamnosus GG, a well-researched strain, has been found effective in reducing gut permeability and inflammation, thus potentially easing the symptoms of UC and improving patient outcomes.
Bifidobacterium
Another critical group of beneficial bacteria is the Bifidobacterium genus, which plays a fundamental role in the digestion of dietary fibers. Through this process, these bacteria help produce short-chain fatty acids (SCFAs), such as butyrate, propionate, and acetate. SCFAs are crucial for the health of colon cells (colonocytes); butyrate, in particular, is a major energy source for these cells and is integral in maintaining the mucosal integrity and proper functioning of the gut.
In the context of UC, the presence of Bifidobacterium in the gut has been associated with numerous positive outcomes, including enhanced digestion and absorption of nutrients, and a strengthened gut barrier which helps reduce the incidence of infection and inflammation.
Faecalibacterium prausnitzii
Faecalibacterium prausnitzii is noteworthy for its strong anti-inflammatory properties within the gut, largely attributed to its ability to produce high levels of butyrate. Studies have shown that individuals with UC often have reduced levels of F. prausnitzii, suggesting that augmenting this bacterium could have therapeutic effects. The anti-inflammatory action of butyrate produced by F. prausnitzii involves not only nourishing the gut lining but also modulating immune responses, which can help in reducing the inflammatory episodes associated with UC.
Why Are They Important?
The strategic enhancement of these beneficial bacteria through dietary choices and probiotic supplementation can play a crucial role in the management of Ulcerative Colitis. By fostering a microbiome rich in Lactobacillus, Bifidobacterium, and Faecalibacterium prausnitzii, patients may experience an alleviation of symptoms through improved gut health, enhanced barrier function, and reduced inflammation. This approach highlights the importance of the microbiome in digestive health and offers a promising avenue for the natural management of UC, complementing traditional medical treatments to improve quality of life for patients living with this challenging condition.
Nutritional Support for Beneficial Bacteria
For individuals living with Ulcerative Colitis (UC), the role of diet extends beyond mere nutrition—it plays a critical part in modulating the gut microbiome, which is a key factor in the disease’s pathology. The gut microbiome consists of trillions of bacteria, some of which can have significant health benefits. Maintaining a healthy balance of these beneficial bacteria is crucial, and one effective way to support their growth is through the consumption of prebiotics.
Understanding Prebiotics
Prebiotics are types of dietary fiber that the human body cannot digest. They serve as food for beneficial gut bacteria, encouraging their growth and activity. This, in turn, can help enhance gut health and immunity, and potentially reduce the inflammatory responses typical of UC. Including prebiotic-rich foods in the diet is a strategic approach to manage UC by supporting the microbiome.
Prebiotic-Rich Foods
Several everyday foods are rich in prebiotics and can be included in a balanced diet to support gut health. Each of these foods contributes to the nourishment of beneficial bacteria, helping to maintain a robust and resilient digestive system.
Garlic, Onions, and Leeks
Garlic, onions, and leeks are part of the allium family and are excellent sources of inulin and fructooligosaccharides (FOS). These compounds are particularly effective at promoting the growth of beneficial Bifidobacteria and Lactobacillus. Both these bacterial strains play crucial roles in gut health, helping to break down food, absorb nutrients, and ward off potential pathogens. Regular consumption of these alliums can help increase the population of these helpful bacteria, contributing to a healthier gut microbiome and potentially easing some UC symptoms.
Bananas and Apples
Bananas and apples are fruits rich in pectin, a type of soluble fiber that not only aids in digestion but also enhances the production of short-chain fatty acids (SCFAs) like butyrate. Butyrate is produced when gut bacteria ferment pectin and other soluble fibers, and it serves as a primary energy source for the cells lining the colon. By nourishing these cells, butyrate helps maintain the integrity of the gut wall and can reduce inflammation, a key benefit for those with UC.
Whole Grains Like Barley and Oats
Whole grains such as barley and oats are valuable sources of beta-glucan. This soluble fiber is known for its wide range of health benefits, including lowering cholesterol and improving heart health. In the context of UC, beta-glucan supports the growth of beneficial gut bacteria, contributing to a balanced microbiome. This support can enhance immune function and decrease gut inflammation, providing relief from some UC symptoms.
Integrating Prebiotics into the Diet
Incorporating these prebiotic-rich foods into a daily diet can be a practical and effective strategy for managing Ulcerative Colitis. For example, starting the day with a bowl of oatmeal topped with sliced bananas or apples can boost your intake of beta-glucan and pectin. Including garlic and onions in cooking not only enhances flavor but also increases your daily intake of inulin and FOS, supporting gut health.
By understanding and leveraging the role of prebiotics in digestive health, individuals with UC can take proactive steps toward managing their condition through dietary choices. This approach, coupled with medical treatment as advised by healthcare providers, offers a comprehensive way to address the symptoms of UC and enhance overall wellbeing.
Supplements for a Healthy Microbiome
In addition to dietary choices, certain supplements can help nurture a healthy microbiome and potentially alleviate UC symptoms:
- Probiotics: Supplements containing live beneficial bacteria can help restore the natural balance of gut microbiota. Specific probiotic formulations designed for UC patients often contain strains like Lactobacillus rhamnosus GG, Bifidobacterium bifidum, and Saccharomyces boulardii. With over 100 clinical trials and a blend formulated to help with Ulcerative Colitis, Visbiome® High Potency Probiotic is a go to probiotic for anyone with Ulcerative Colitis.
- Prebiotics: Supplements such as inulin, fructooligosaccharides (FOS), and galactooligosaccharides (GOS) can help increase the levels of beneficial gut bacteria.
- Butyrate supplements: Butyrate has been shown to have anti-inflammatory effects on the colon, and supplementing with butyrate can help in cases where dietary fiber intake is insufficient.
Foods to Avoid for Ulcerative Colitis
High-Sugar Foods and Drinks
Sugars, particularly refined sugars found in sodas, candies, and many processed foods, are a major culprit in disrupting gut health. These sugars provide a rapid energy source for harmful bacteria and yeasts, promoting their growth and activity. This can lead to an overproduction of gases and toxins which can further inflame the gut lining, worsening UC symptoms. Additionally, a high-sugar diet can lead to an imbalance in the gut microbiota, known as dysbiosis, which impairs the gut barrier function and can trigger or worsen inflammatory processes in the colon.
Processed and Refined Foods
Processed foods are typically high in additives and preservatives which can have various negative effects on gut health. These substances can alter the gut’s pH and the composition of the gut microbiome, making the environment more favorable for pathogenic bacteria than for beneficial microbes. Common additives like emulsifiers and artificial sweeteners have been shown in studies to interfere with microbial balance and increase gut permeability, potentially triggering inflammatory responses in individuals with UC.
Red Meat and High-Fat Foods
Diets high in red meat and saturated fats can also adversely affect the microbiome. These foods increase the production of bile acids in the gut; excessive bile acids can be detrimental to certain beneficial bacteria, such as Bifidobacterium, which thrive in lower bile environments. Furthermore, high-fat diets have been linked to increased levels of inflammation and may exacerbate the symptoms of UC. The fats often found in fast food and deep-fried items can be particularly challenging, as they are difficult to digest and can stimulate the immune system to act more aggressively, which is problematic for those with inflammatory bowel diseases.
Conclusion
The gut microbiome plays a significant role in the pathology of Ulcerative Colitis, influencing both the onset and progression of the disease. Through strategic dietary and supplement choices aimed at nurturing beneficial bacteria and their growth, individuals with UC can potentially mitigate symptoms and improve their quality of life. As research continues to evolve, it becomes increasingly clear that a holistic approach involving diet, lifestyle, and medical treatment is essential for managing UC and other inflammatory bowel diseases effectively.
If you’re interested in boosting your beneficial gut bacteria naturally without relying on supplements, be sure to read 9 Fermented Foods for Improving Ulcerative Colitis and Gut Health.