In the ongoing battle against ulcerative colitis (UC), a chronic and often debilitating inflammatory bowel disease, patients and healthcare providers are constantly on the lookout for effective treatment strategies that extend beyond conventional medical interventions. Enter cognitive-behavioral therapy (CBT), a psychological intervention that has shown promise in not only managing the psychological impacts of chronic illnesses but also in potentially alleviating the physical symptoms associated with UC.
The Psychological Burden of Ulcerative Colitis
Ulcerative colitis affects millions worldwide, with its hallmark symptoms of abdominal pain, frequent bowel movements, and fatigue. But the impact of UC isn’t limited to physical symptoms. The chronic unpredictability of flare-ups contributes to significant psychological distress. Patients often experience heightened levels of anxiety and depression, which can exacerbate their physical condition. The constant concern over potential flare-ups and the need for frequent access to bathrooms can lead to social withdrawal and a diminished quality of life.
Moreover, the emotional toll of managing a long-term illness such as UC can strain personal relationships and impact professional life, creating a cycle of stress that can further aggravate the disease. Many patients report feeling isolated because of their symptoms, which can be difficult for others without the disease to fully understand. Managing these multifaceted challenges requires a comprehensive approach that addresses both the psychological and physical aspects of the disease.
Cognitive-Behavioral Therapy: More Than Just a Mental Health Tool
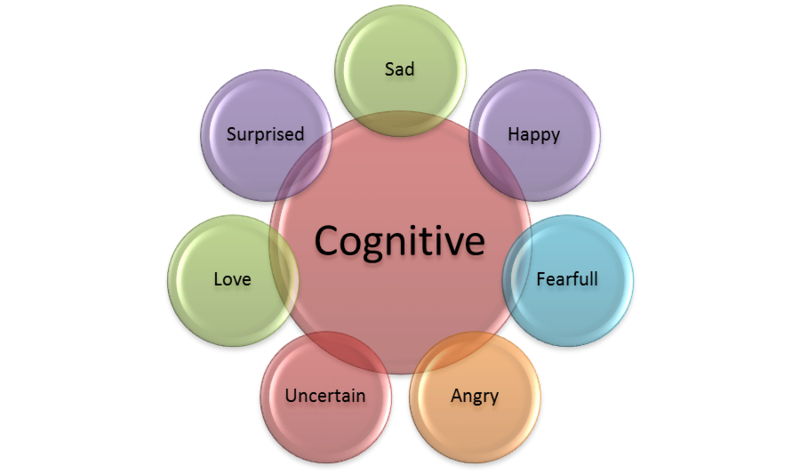
Traditionally used to treat anxiety, depression, and other mental health disorders, cognitive-behavioral therapy is now making strides in the realm of physical health, particularly chronic diseases like ulcerative colitis. CBT operates on the premise that changing maladaptive thoughts and behaviors can significantly influence one’s emotional regulation and physical health. This approach is based on the idea that negative thought patterns and behaviors can exacerbate physical symptoms and that altering these patterns can lead to improved management of chronic conditions.
CBT is particularly beneficial for UC patients, who often deal with the stress and anxiety that can trigger or worsen their symptoms. By integrating techniques aimed at reducing stress and promoting positive thought patterns, CBT helps patients gain better control over their emotional responses to their illness. This, in turn, can lead to a reduction in flare-ups and an improvement in overall quality of life, illustrating the powerful connection between mental health and physical well-being in the context of chronic disease management.
Cognitive-Behavioral Therapy and Ulcerative Colitis: The Connection
Research indicates that stress and anxiety can trigger or worsen UC flare-ups. CBT helps patients develop coping strategies to manage stress and modify the negative thought patterns that can escalate into physical symptoms. By teaching relaxation techniques, stress management skills, and ways to challenge irrational or harmful thoughts, CBT empowers UC patients to take a more active role in managing their condition.
Evidence Supporting CBT in UC Management
A significant study published in the “Journal of Psychosomatic Research” demonstrates the benefits of cognitive-behavioral therapy for patients with ulcerative colitis. According to the findings, UC patients who underwent CBT experienced not only a reduction in psychological distress but also reported a noticeable decrease in the severity of their gastrointestinal symptoms. These results underline the potential of mental health therapy as an integral part of comprehensive UC treatment plans, suggesting that addressing psychological well-being can directly influence and improve physical health outcomes. This study reinforces the importance of a holistic approach in the management of UC, integrating both psychological and physiological healthcare strategies to enhance patient care and quality of life.
Stress Management and Natural Supplements in Ulcerative Colitis
Patient Perspectives
Many patients with ulcerative colitis have embraced cognitive-behavioral therapy as a complementary approach alongside their medical treatments. Sarah, a 34-year-old UC patient, attests to the benefits she has experienced from integrating CBT into her treatment plan. She explains, “CBT helped me manage my stress and put my disease in perspective. It’s not a cure, but it’s a tool that helps me cope better with the challenges of UC.” Her testimony highlights the effectiveness of CBT in providing patients with strategies to better handle the psychological stress that often accompanies chronic illness, thereby improving their overall ability to manage the condition.
The Role of Healthcare Providers
Gastroenterologists and mental health professionals are increasingly advocating for a multidisciplinary approach to the treatment of ulcerative colitis. This strategy encompasses a blend of medical and psychological therapies to address the full spectrum of the disease. Dr. Emily Tran, a gastroenterologist specializing in inflammatory bowel diseases, emphasizes the benefits of this comprehensive approach. “We see significant improvements in patients who participate in CBT. It’s an essential part of our holistic approach to managing UC, which includes diet, medication, and mental health,” she stated. This endorsement highlights the importance of integrating cognitive-behavioral therapy into the standard treatment regimen, recognizing its role in enhancing patient outcomes by tackling both the physical and psychological aspects of UC.
Embracing a Holistic Future in Ulcerative Colitis Management
As ulcerative colitis continues to challenge patients with its cyclical pattern of remission and flare-ups, cognitive-behavioral therapy stands out as a beacon of hope. This therapy offers patients robust strategies for managing the psychological toll of living with a chronic illness and has shown potential in alleviating the physical symptoms as well. With continued research and enhanced patient education, CBT is poised to become a standard adjunct therapy in the management of UC. This integration could significantly transform the treatment landscape for this complex disease, offering a more holistic approach that addresses both the mental and physical aspects of UC.