Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. It is characterized by the inflammation and ulceration of the innermost lining of the colon, leading to symptoms such as abdominal pain, urgent and bloody diarrhea, and significant disruption to everyday life. Understanding UC requires an exploration of its pathophysiology, symptoms, diagnosis, treatment options, and the impact it has on individuals’ lives.
Pathophysiology
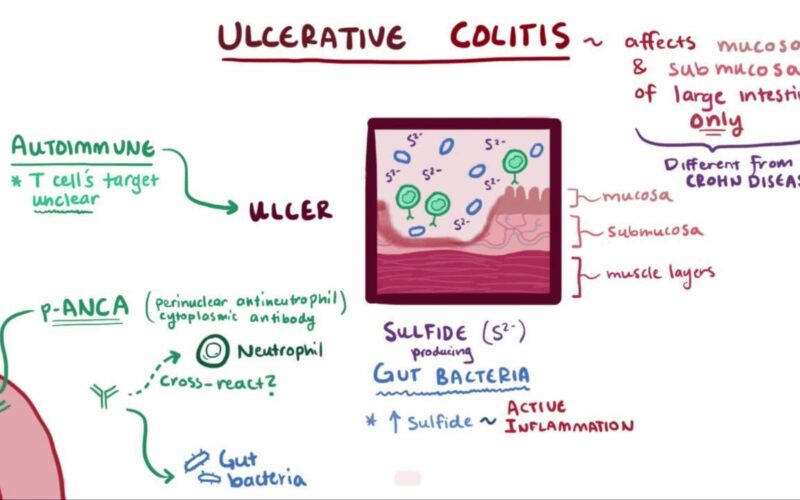
Ulcerative colitis is an autoimmune condition, where the body’s immune system mistakenly targets its own intestinal tissues, causing inflammation and tissue damage. This process typically starts in the rectum and may extend continuously to involve the entire colon. Unlike Crohn’s disease, another type of IBD that can affect any part of the gastrointestinal tract and penetrate deeper into the bowel walls, UC affects only the superficial layers (mucosa and submucosa) of the colon.
The exact cause of UC is still not well understood, but it is believed to result from a complex interaction of genetic, environmental, and immune factors. Several genes have been linked to an increased risk of developing UC, suggesting a hereditary component. Environmental factors such as diet, stress, and the gut microbiome (the community of microorganisms in the intestines) also play crucial roles. For instance, a diet high in saturated fats and sugar but low in fiber has been associated with an increased risk of UC.
Ulcerative Colitis Symptoms
Ulcerative colitis manifests through a variety of symptoms that can significantly affect a person’s quality of life. These symptoms are primarily gastrointestinal but can also include systemic effects that impact other parts of the body.
Gastrointestinal Symptoms
- Diarrhea: This is one of the most common symptoms of UC, often severe and bloody. The presence of blood is due to the ulcers or sores that form in the colon’s lining, which bleed as they become aggravated by the passage of stool. The stool may also contain pus or mucus, a sign of inflammation and infection within the colon.
- Abdominal Pain and Cramping: UC often causes significant discomfort, with pain usually concentrated in the lower abdomen. This pain results from inflammation and ulceration in the colon which increases during the bowel movements. The pain can vary in intensity and may be constant or sporadic.
- Urgency to Defecate: This symptom is characterized by a sudden, compelling need to have a bowel movement. It occurs because the inflamed colon becomes hypersensitive and reacts to even small amounts of stool by trying to expel it quickly.
- Rectal Pain: Pain and bleeding from the rectum are common in UC due to inflammation and ulceration at the end of the colon. Bleeding can range from light to severe, often noticed as bright red blood on toilet paper or in the toilet bowl.
Systemic Symptoms
- Weight Loss and Fatigue: These symptoms occur because the inflamed colon does not absorb nutrients effectively, leading to a deficiency in calories and essential nutrients. Fatigue may also result from anemia and the chronic nature of the disease, which can tax the body’s energy reserves.
- Anemia: Chronic blood loss from damaged mucosal linings in the intestine often leads to iron-deficiency anemia. This condition reduces the number of red blood cells necessary to carry oxygen throughout the body, leading to symptoms like fatigue, weakness, and pallor.
Extraintestinal Symptoms
Ulcerative Colitis is not limited to the colon; it can have systemic effects, known as extraintestinal manifestations, which include:
- Arthritis: The most common extraintestinal symptom, arthritis can affect various joints, causing pain, swelling, and stiffness. This occurs because the inflammation in the colon can trigger the immune system to attack the joints.
- Skin Problems: Conditions like erythema nodosum, which causes tender red bumps, primarily on the shins, and pyoderma gangrenosum, a rare condition that causes painful, necrotic ulcers, are associated with UC.
- Eye Inflammation: Conditions such as uveitis, which causes inflammation of the uvea (the middle layer of the eye), can lead to redness, pain, and blurred vision. This is another immune-mediated symptom reflecting the systemic nature of UC.
- Liver Disorders: Some individuals with UC may develop liver conditions such as primary sclerosing cholangitis, which involves inflammation and scarring of the bile ducts. This can lead to liver dysfunction and, in severe cases, liver failure.
These symptoms and their varied manifestations underscore the complexity of ulcerative colitis and the importance of comprehensive management strategies that address both the gastrointestinal and systemic components of the disease. Managing UC effectively requires a multifaceted approach tailored to the individual’s specific symptoms and overall health.
10 Common Symptoms of Ulcerative Colitis You Should Know
Diagnosing Ulcerative Colitis: A Comprehensive Approach
The diagnosis of ulcerative colitis (UC) is a multi-step process that incorporates clinical evaluation, laboratory tests, and imaging to ensure accuracy and to differentiate UC from other conditions with similar symptoms. Here’s a detailed look at the diagnostic steps and tools involved:
Clinical Evaluation
- Medical History: The first step in diagnosing UC involves a detailed discussion about the patient’s symptoms, duration of symptoms, family history of IBD or other autoimmune diseases, and any medications or lifestyle factors that may influence their condition.
- Physical Examination: A physical exam focuses on assessing the abdominal area for pain, tenderness, or swelling and checking for signs of pallor (which could suggest anemia) or other physical indicators of chronic illness.
Laboratory Tests
- Blood Tests: Blood samples are analyzed to check for anemia, which could indicate chronic blood loss typical in UC. They also measure inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), which tend to be elevated in active UC. Blood tests can help assess the overall health and to rule out other causes of symptoms like infections.
- Stool Tests: These tests are crucial for differentiating UC from infectious causes of diarrhea (such as bacterial, viral, or parasitic infections). They may also detect the presence of white blood cells in the stool, which indicates inflammation of the intestines.
Calprotectin Levels: A Key Indicator in Managing Ulcerative Colitis
Endoscopic Examination
- Colonoscopy: This is the gold standard test for diagnosing UC. During a colonoscopy, a flexible tube equipped with a camera (colonoscope) is inserted into the rectum to visually examine the entire colon and rectum. The key advantage of a colonoscopy is its ability to directly observe the characteristic patterns of inflammation and ulceration that are typical in UC. Moreover, it allows the gastroenterologist to perform biopsies—taking small tissue samples from the lining of the colon—which are crucial for confirming the presence of typical histopathological features of UC.
Imaging Studies
- X-rays: While not routinely used for diagnosing UC, plain abdominal X-rays can be helpful in emergency settings to check for complications like toxic megacolon or colonic perforation.
- CT Scans: Computed tomography (CT) scans provide a detailed, cross-sectional image of the abdomen, helping to assess the extent of colonic inflammation and to rule out complications such as abscesses or other sources of abdominal pain.
- MRI: Magnetic resonance imaging (MRI) of the abdomen can be used in specific circumstances, particularly to assess the small intestine or to evaluate perianal disease, which can sometimes accompany UC.
The combination of these diagnostic tools allows for a comprehensive evaluation of UC, aiding not just in diagnosis but also in monitoring the disease progression and response to treatment. Each tool provides unique insights, and together they furnish a complete picture that guides effective management of the disease.
Ulcerative Colitis Treatment
The treatment for ulcerative colitis is primarily aimed at inducing and maintaining remission, healing the colon’s lining, and enhancing the quality of life. Contemporary medical treatments have shown some effectiveness in managing UC, and there is growing interest in the potential benefits of natural remedies as supportive therapies. These often come with unwanted side effects, but the main treatment options doctors prescribe include:
Aminosalicylates
Function: Aminosalicylates are often the first line of treatment for mild to moderate ulcerative colitis. These medications work by reducing inflammation directly at the lining of the colon. They are particularly effective in preventing flare-ups and maintaining remission in UC.
Side Effects: While generally well-tolerated, aminosalicylates can have side effects such as nausea, headaches, abdominal pain, and rash. In rare cases, they may cause kidney problems, pancreatitis, or allergic reactions, which necessitate monitoring by healthcare providers.
Corticosteroids
Function: Corticosteroids are powerful anti-inflammatory drugs used to manage severe flares of ulcerative colitis. They provide quick relief of symptoms and are effective in reducing inflammation throughout the body, not just in the colon.
Side Effects: The side effects of corticosteroids are significant, especially with long-term use, and include increased risk of infections, osteoporosis, high blood pressure, diabetes, weight gain, mood swings, and cataracts. Due to these potential risks, they are recommended for short-term use and not as a maintenance therapy.
Immunomodulators
Function: Immunomodulators such as azathioprine and mercaptopurine lower the immune system’s activity, thereby reducing inflammation. These drugs are used for maintaining remission in UC and are suitable for long-term use in managing chronic symptoms.
Side Effects: Because immunomodulators suppress the immune system, they increase the risk of infections. Other potential side effects include liver toxicity, pancreatitis, nausea, and a slight increase in the risk of lymphoma. Regular blood tests are required to monitor the effects of these drugs on liver function and white blood cell counts.
Biologics
Function: Biologics are targeted therapies that block specific molecules involved in the inflammatory process. Drugs like infliximab, adalimumab, and vedolizumab are designed to target tumor necrosis factor (TNF) or specific integrins, which are key players in the inflammatory pathways that cause UC symptoms.
Side Effects: The side effects of biologics can include increased risk of serious infections, reactivation of latent tuberculosis, potential for allergic reactions, and rarely, lymphoma. Patients on biologic therapies are monitored closely for these complications.
JAK Inhibitors
Function: Janus kinase (JAK) inhibitors, such as tofacitinib, represent a newer class of oral medications used to treat UC. They work by blocking Janus kinase enzymes involved in the inflammation process, which helps reduce the activity of the immune system specifically impacting the pathways that exacerbate UC.
Side Effects: JAK inhibitors can lead to an increased risk of blood clots, elevated cholesterol levels, and liver enzyme abnormalities. They can also increase the risk of infections, including serious viral infections. Close monitoring and regular blood tests are essential to manage these risks effectively.
The choice of medication for treating ulcerative colitis depends on the severity of the disease, the specific symptoms, and the overall health of the patient. While these medications can significantly improve quality of life and disease outcomes, their potential side effects require careful consideration and regular monitoring by healthcare professionals. This balanced approach ensures that the benefits of treatment are maximized while minimizing adverse effects.
Natural Ulcerative Colitis Treatments
As interest in holistic health management grows, many individuals with ulcerative colitis are increasingly turning to natural remedies. These remedies can complement or, in some cases, serve as alternatives to conventional medications, under the guidance of healthcare professionals.
Probiotics
Function: Probiotics help restore the natural gut flora disrupted by Ulcerative Colitis, which may enhance digestive health and reduce inflammatory responses in the colon. These can be consumed in supplement form, but incorporating fermented foods into your diet is an excellent way to naturally boost your probiotic intake. For further details on how to enhance gut health and manage ulcerative colitis through diet, consider exploring resources like the article “9 Fermented Foods for Improving Ulcerative Colitis and Gut Health.”
Specific Strains: Lactobacillus, Bifidobacterium, and Saccharomyces boulardii are commonly used for their potential benefits in reducing intestinal inflammation and maintaining remission.
Herbal Remedies
- Turmeric (Curcumin): Curcumin, the active compound in turmeric, has potent anti-inflammatory properties that may help reduce colonic inflammation. It inhibits key inflammatory cytokines and enzymes, such as COX-2 and 5-LOX.
- Ginger: Known for its gastrointestinal benefits, ginger can help reduce inflammation and alleviate symptoms like cramping and nausea.
- Aloe Vera: The gel from aloe vera leaves can soothe the gut lining and reduce inflammation, potentially easing UC symptoms.
- Qing Dai (Indigo Naturalis): This traditional Chinese medicine has shown promise in several small studies for its efficacy in treating UC. Qing Dai exhibits anti-inflammatory effects and has been used in the form of enemas or oral capsules to help induce and maintain remission in UC.
- Boswellia Serrata: Also known as Indian frankincense, Boswellia has anti-inflammatory properties that may help manage chronic inflammatory conditions like UC. It works by inhibiting leukotriene synthesis, which is involved in the inflammatory process. Learn more about Boswellia Serrata here: Boswellia Serrata’s Potential in Treating Ulcerative Colitis
- Slippery Elm: The bark of the slippery elm tree forms a gel-like substance when mixed with water, which coats the lining of the colon, potentially soothing irritation and reducing inflammation.
Dietary Adjustments
Function: Tailoring the diet is crucial in managing UC symptoms and preventing flare-ups.
- Whole Foods Diet: Emphasizing fresh fruits, vegetables, lean proteins, and whole grains can support overall health and reduce inflammation. Processed foods, which often contain additives and high levels of sugar, should be avoided.
- Elimination Diet: Identifying and avoiding trigger foods is a personalized strategy that can be highly effective. Common triggers include dairy, gluten, high-fat foods, and spicy foods.
Other Natural Approaches
- Fish Oil: Rich in omega-3 fatty acids, fish oil supplements can help reduce inflammation. Omega-3s are known to inhibit the production of inflammatory eicosanoids and cytokines.
- Prebiotics: These non-digestible fibers promote the growth of beneficial gut bacteria, enhancing the effects of probiotics and supporting gut health.
- Mind-Body Therapies: Techniques such as meditation, yoga, and tai chi can help manage stress, which may exacerbate symptoms of UC.
Natural remedies offer a range of options for individuals looking to manage ulcerative colitis holistically. While these treatments can be effective, they should be pursued in consultation with healthcare providers to ensure they are used safely and effectively in conjunction with, or as an alternative to, traditional medical treatments. As research evolves, the potential for integrating these natural therapies into mainstream UC management continues to expand, providing hope and diverse options for those affected by this challenging condition.
Surgery
Surgical intervention should be considered an absolute last resort for managing ulcerative colitis. It becomes a necessity only in cases where medications fail to control the disease adequately, or if the patient experiences severe complications such as significant bleeding, perforation of the colon, or a high risk of cancer. The most radical surgical option, a proctocolectomy, involves the complete removal of the colon and rectum. While this procedure can effectively eliminate UC, it requires the patient to live with an ileostomy bag or a surgically constructed internal pouch, significantly impacting their lifestyle.
In summary, the treatment of UC typically involves a strategic combination of medical therapies and, increasingly, supportive natural treatments. Many patients find these combined approaches beneficial for symptom management. However, any treatment plan, especially one considering surgical options, should be carefully guided by healthcare professionals to ensure it is tailored to meet the specific needs and circumstances of the individual.
Living with Ulcerative Colitis
Living with ulcerative colitis presents a multitude of challenges that extend beyond physical symptoms, deeply affecting the emotional, social, and psychological aspects of a person’s life. The chronic nature of UC and the unpredictable timing of flare-ups can make daily life difficult and stressful.
Emotional and Psychological Impact
The ongoing struggle with UC can lead to significant emotional distress. Many individuals with UC report feelings of anxiety and depression, stemming not only from the disease itself but also from its management challenges. The urgency and frequency of bowel movements, a hallmark symptom of UC, can lead to embarrassment and anxiety, particularly in social or work environments. This can cause individuals to withdraw from social interactions and avoid activities they previously enjoyed, leading to isolation and impacting their mental health.
Moreover, the unpredictability of flare-ups can lead to a constant state of vigilance and anxiety about when and where symptoms may occur, complicating planning and participation in everyday activities. This can exacerbate stress, which in turn can trigger more frequent or severe flare-ups, creating a vicious cycle.
Social Well-Being
The impact of UC on social interactions can be profound. The need for frequent bathroom access can inhibit social activities, travel, and professional opportunities. People with UC might feel they need to plan their activities meticulously around their condition, with a constant awareness of the nearest bathroom facilities. This can strain relationships and reduce the quality of life, making it hard to feel relaxed in social settings.
Managing Symptoms with Diet and Lifestyle
Despite these challenges, many effective strategies can help manage UC symptoms and improve quality of life:
- Dietary Adjustments: During flare-ups, a low-fiber diet can help reduce bowel movements and minimize abdominal pain. This involves limiting foods such as raw fruits and vegetables, whole grains, and nuts, which can exacerbate symptoms. Many patients also benefit from identifying and avoiding their specific food triggers, which can vary widely among individuals with UC. Keeping a food diary can be helpful in tracking which foods exacerbate symptoms.
- Stress Management: Techniques such as meditation, yoga, and regular exercise are not only beneficial for overall health but also particularly effective in managing stress related to chronic illness. Meditation can help center the mind and reduce anxiety, while yoga combines physical movement with breath control exercises, promoting relaxation and improving physical fitness. Regular exercise helps improve mood and maintain physical health, which can be compromised in UC. For more information about stress management be sure to read Stress Management and Natural Supplements in Ulcerative Colitis.
- Support Systems: Engaging with support groups, either in person or online, can provide emotional comfort and practical advice, helping individuals feel less isolated. These communities can offer valuable support from others who understand the challenges of living with UC.Take the time to read The Emotional Impact of Living with Ulcerative Colitis to learn how support systems can go a long way in helping you live a better life with Ulcerative Colitis.
By integrating these management strategies into daily life, individuals with UC can find better ways to cope with the disease, reducing its impact on their emotional, social, and psychological well-being. It’s important for patients to work closely with their healthcare providers to develop a comprehensive management plan that addresses both the physical and emotional aspects of the disease.
Conclusion
In conclusion, ulcerative colitis is a complex and challenging condition, but with ongoing advancements in medical research and comprehensive management strategies, individuals living with UC can lead fulfilling lives. Research plays a crucial role in unraveling the intricate mechanisms behind UC and paves the way for the development of innovative treatments that target the specific pathways involved in the disease process. As understanding deepens, treatments become more refined, offering better control of symptoms and improved quality of life for patients.
Effective management of Ulcerative Colitis involves a holistic approach that combines medical treatments tailored to individual needs with lifestyle adjustments. Medications, including aminosalicylates, corticosteroids, immunomodulators, biologics, and in severe cases, surgery, form the backbone of medical treatment strategies aimed at reducing inflammation and maintaining remission. Alongside medical treatment, dietary modifications and stress reduction techniques such as meditation, yoga, and regular physical activity play a critical role in managing the daily challenges of the disease.
Moreover, the support from healthcare professionals, alongside the emotional and practical support from family, friends, and peers, is indispensable. This network not only helps in the direct management of the condition but also in coping with the psychological impacts of living with a chronic illness.
Despite the considerable challenges posed by UC, many affected individuals continue to lead active, productive lives. The key lies in the effective integration of medical care, lifestyle management, and support networks, all tailored to meet the unique needs of each patient. With the right approach, the impact of UC can be significantly mitigated, allowing individuals to pursue their goals and enjoy a high quality of life.